Hospitals are under increasing pressure to manage costs, streamline operations, and deliver more consistent patient care, all without adding administrative burden to frontline staff. One often overlooked area ripe for improvement is the PAR room.
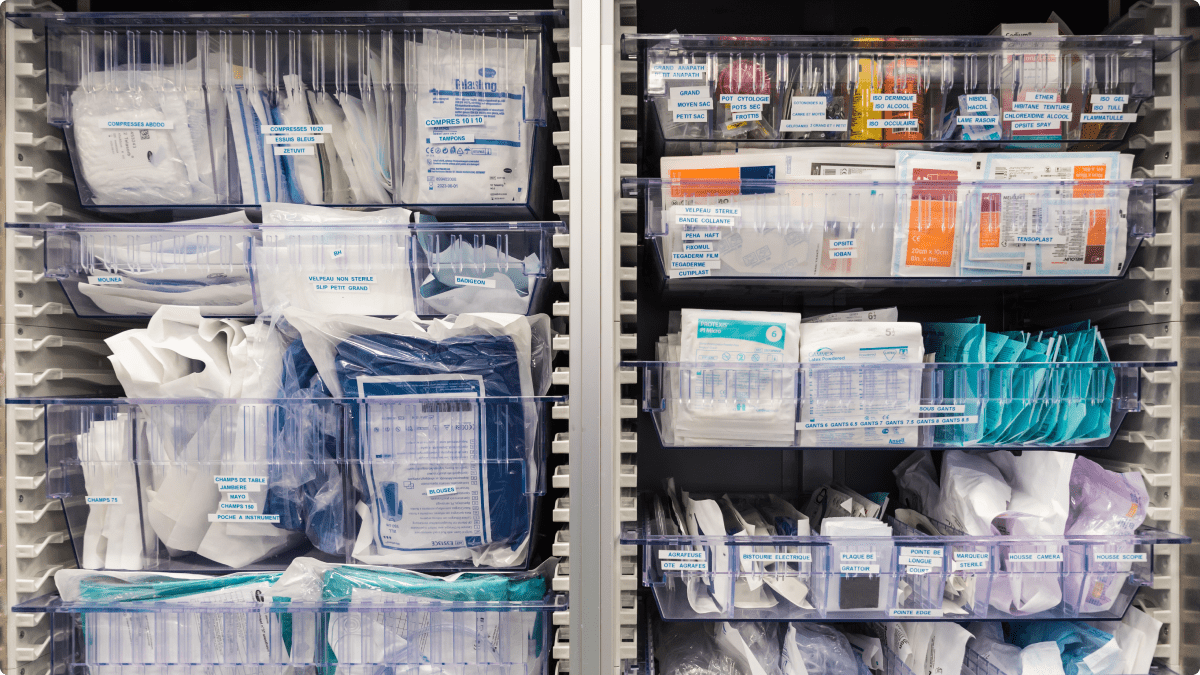
Short for Periodic Automatic Replenishment, PAR rooms are where hospitals store the everyday clinical supplies needed to keep care moving. Most large health systems manage hundreds of these rooms, each holding hundreds of SKUs. While the term “automatic” is in the name, the reality in many hospitals is anything but.
Today, hospitals are rethinking how PAR rooms function. The shift is toward automation that reduces manual work, increases inventory accuracy, and ensures supplies are restocked before they run out. It is part of a broader move toward AI-powered supply chain modernization, where automation supports both operational and clinical goals.
Why PAR Rooms Deserve a Closer Look
Supply chain teams are already deeply familiar with the structure and function of PAR rooms. What’s often underestimated, however, is how much variation and friction exists in their day-to-day replenishment processes. PAR rooms are meant to support just-in-time availability of hundreds of routine clinical supplies. Yet in many hospitals, practices still rely on disconnected scanning routines, staff memory, or manual intervention from nurses who are already stretched thin.
This variability leads to inconsistent performance, and it’s a root cause of stockouts, overordering, and supply waste. The opportunity isn’t about redefining what a PAR room is—it’s about modernizing how it operates across hundreds of decentralized environments. For hospitals managing thousands of SKUs systemwide, even small inefficiencies add up quickly. Automation is the lever to standardize performance and relieve the invisible burden these rooms place on staff.
The Cost of Manual Replenishment
Manual processes carry real consequences. According to Becker’s Hospital Review, inefficiencies in hospital supply chains cost health systems an estimated $25 billion annually in waste. Much of this waste originates in places like PAR rooms, where overstocking “just in case” leads to expired products, hoarding, and poor space utilization.
Understocking or delayed restocking leads to stockouts that can delay care, trigger emergency orders, or force staff to search other units for missing items. Nurses, already facing burnout and staffing shortages, often report spending up to 20 percent of their time on supply-related tasks that do not require clinical training.
As stockouts become more preventable with AI, automation plays a critical role in reducing inefficiencies while maintaining clinical readiness.
Why Now Is the Time to Redesign Replenishment Models
Hospital supply chains are under more scrutiny than ever, not just from finance and operations teams, but from clinicians who feel the pain of supply uncertainty daily. The drive for automation in PAR rooms reflects a broader shift: moving from reaction to precision. Health systems are no longer content to rely on static reorder points or sporadic cycle counts. They want dynamic replenishment informed by real usage data, captured in real time.
This redesign is not just a technology upgrade—it’s a supply chain strategy decision. It enables teams to free up clinical labor, improve accuracy at scale, and create more resilient inventory systems that can adjust automatically as patient volumes shift.
From Two-Bin to Touchless: Evolving the Model
The two-bin method—one bin in use, one as backup—has been a mainstay in hospitals for decades. When the first bin empties, a scan or visual cue initiates restocking. It is simple but limited by its reliance on staff availability and manual confirmation.
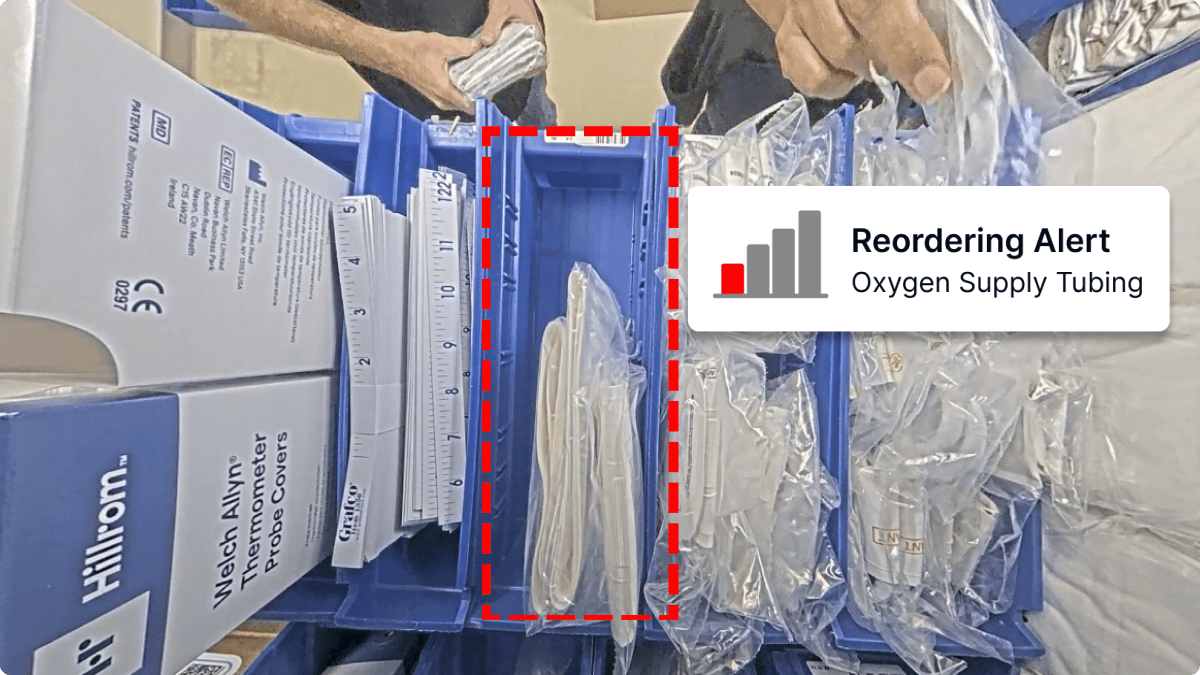
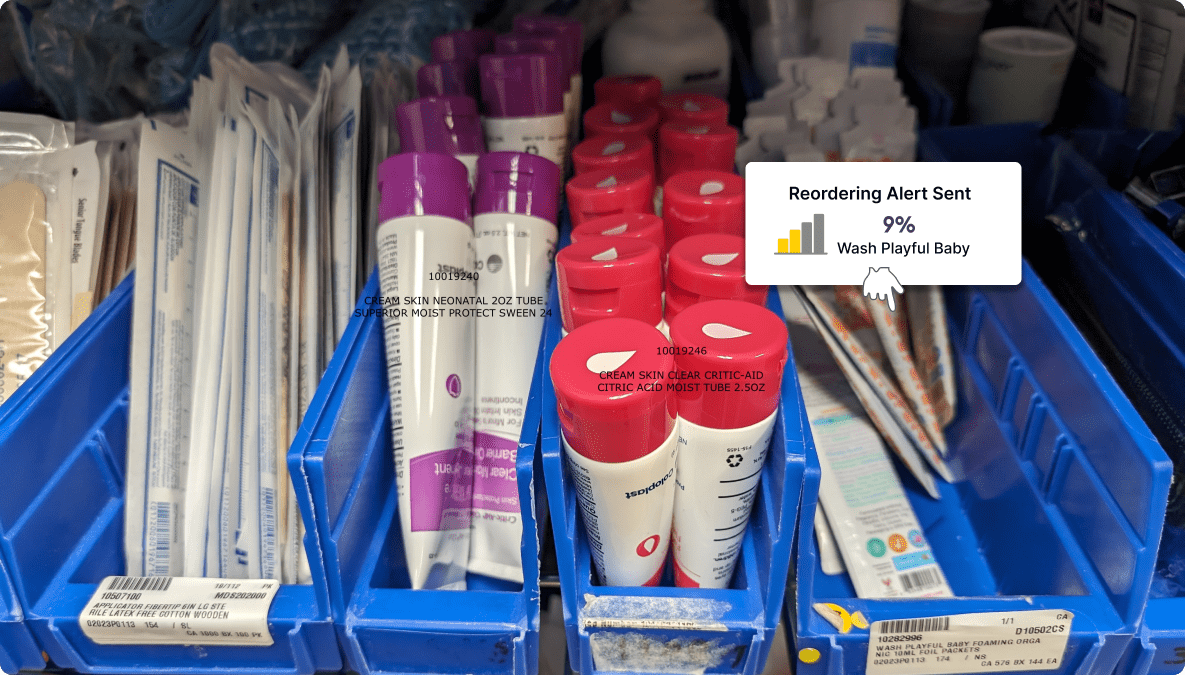
Today’s systems build on that foundation by using real-time data, often from sensors or cameras, to detect when supplies are low before bins are empty. This enables earlier, more accurate replenishment with fewer manual steps. Hospitals adopting these data-driven models report reduced inventory volumes, fewer last-minute restocks, and more consistent ordering. Clinicians spend less time on inventory tasks and more time on patient care.
Making Automation Work Inside the Supply Chain Workflow
Too often, automation initiatives fail because they are built for the wrong end users. PAR room automation should serve the supply chain team first—supporting efficient restocking, accurate demand planning, and integration with purchasing systems. If it adds steps or complexity for nurses or materials management staff, it creates friction.
The most effective systems collect data passively and route actionable information directly to supply chain leads. Alerts should drive system-side workflows like requisition creation or PO triggers, not just notify someone to take manual action. Automation that reinforces internal accountability is more likely to stick and scale, particularly when aligned with zero-touch inventory strategies.
Data That Drives Better Decisions
PAR room automation is not just about visibility. It also produces high-value insights such as usage trends by location, patterns of underutilization, and tracking of critical supplies. These insights help supply chain leaders optimize stocking levels, reduce SKU redundancy, and make more informed procurement decisions. In a cost-constrained environment, data-backed adjustments are essential for long-term sustainability.
Evaluating the Right Automation Fit for Your System
Not all inventory automation tools are built for PAR room use at scale. Health systems should look for solutions that offer passive, real-time tracking without disrupting existing workflows. Systems must integrate with enterprise platforms—ERP, EHR, supply chain—to avoid creating yet another data silo.
More importantly, they should deliver SKU-level visibility, configurable restocking thresholds, and scalable architecture. Whether rolling out across 10 rooms or 1,000, the platform must maintain performance and precision. Security, privacy, and compliance are table stakes, but the differentiator lies in how much actionable intelligence the system provides.
Moving Forward
Hospitals do not need to overhaul their infrastructure to begin automating PAR rooms. Many systems are designed to layer onto existing shelving and layouts with minimal disruption. Most implementations begin gradually, using performance data to guide further rollout.
PAR room automation addresses one of the most persistent inefficiencies in hospital operations: fragmented inventory practices that burden staff and inflate costs. By modernizing this core function, hospitals gain real-time visibility, reduce waste, and improve operational readiness.
As the healthcare industry continues to push for smarter systems, workforce relief, and cost accountability, PAR room automation is no longer optional. It is foundational to a more connected, resilient supply chain.
Want to explore what PAR room automation could look like in your hospital? Request a consultation with our experts. Learn more about AI for Chooch Autonomous AI for healthcare inventory management.